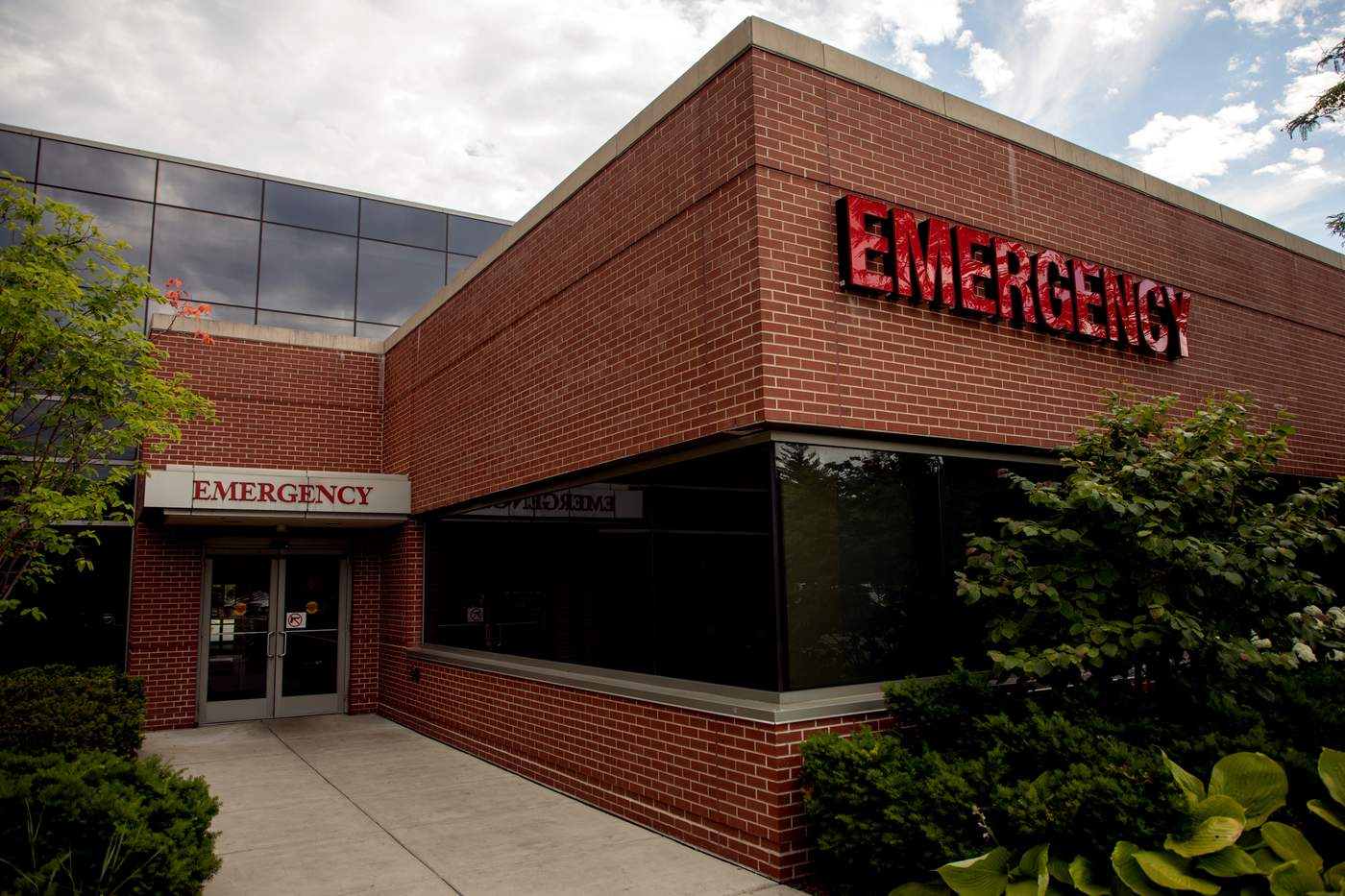
At West Suburban Medical Center in Oak Park, shooting victims come through the emergency room doors, on average, every few days.
The mid-sized community hospital is across the street from Chicago’s Austin neighborhood, where more than 500 people were shot last year and at least 130 people have been shot so far this year.
If an ambulance picks up a shooting victim, chances are paramedics would rush that person to one of Chicago’s big trauma centers, which have around-the-clock specialists on standby.
But at West Suburban, the shooting victims that the doctors see are almost always on a walk-in basis.
Dr. Kip Adrian, chairman of the department of emergency medicine at West Suburban, said his team has treated about 300 shooting victims over the past three years, with about 40 percent of them being sent on to trauma centers.
Adrian said traces of gun violence also show up in more routine evaluations: “Literally every shift you see somebody with belly pain or [someone who’s] here for some other evaluation besides trauma ... and you go to examine them, and they have big scars from previous surgeries related to some sort of violent incident.”
As part of WBEZ’s ongoing project on gun violence in Chicago, Adrian talked about what it’s like to treat shooting victims and how he sometimes gets a chance to intervene with patients to try to prevent violent retaliation. He also talked about the difficult responsibility of telling family and friends that their loved one has died.
Between two worlds
Kip Adrian: It’s really a fascinating area where the hospital sits.... West Suburban Medical Center is on Austin Avenue ... just a little bit north of Lake Street, and it straddles two very, very different communities. To the west is Oak Park and then River Forest, both communities which I think would be considered more affluent…. And then if you go east, you head into the Austin neighborhood, which quickly becomes a fairly depressed area, socio-economically, and is really one of the hubs for gun violence in the city.
We tend to see young men, typically African-American ... as [there’s] a large African-American community that we live next to ... that tend to be the victims….
Somewhere between ages 14 to 25 I’d say is really the spread of the most common victims that we see.... Certainly we’ve seen young kids come through, and older folks as well … but that tends to be the majority of patients.
(Andrew Gill/WBEZ)
‘It is always a walk-in for us’
Adrian: Unless it’s a very mild injury, EMS bypasses us to take [patients] to one of the [Level I] trauma centers … so we carry that volume of 300 over three years, and that’s almost entirely people who simply brought themselves to our doors.
We see people literally pushed out of cars…. We see people who walk in shot, people carried in shot…. A lot of times, you’ll see cars that are sprayed down with bullets, bullet holes all over the place ... and you have literally no warning to deal with that.
You never know what environment is surrounding these patients. You don’t know if somebody is following them. You don’t know who the people are who brought them in. You don’t know if there’s a level of intoxication. You don’t know if they’re carrying weapons. Everything’s unknown in that situation.
To protect the staff and the other patients who are here, there is a lock-down protocol. What that involves is … our security team will literally lock down the department where nobody is allowed in or out without being cleared through security.
Preventing retaliation
Adrian: There’s a spectrum [of reactions to being shot]. And it just depends on the person…. Certainly [shooting victims] show up in shock, and refusing to accept that they’ve been shot.
A lot of times, there is extreme anger. And they want a phone. And they want to call whoever it is they want to call. And they make no bones about it that there is going to be retaliation. And that’s a really scary proposition....
Part of the lock down protocol is that it’s really only immediate family that’s let back. It’s not friends or acquaintances….
Certainly it’s within their right to want to talk to people…. I’ll be honest, I’ve certainly delayed getting phones to people who are in that state of mind…. Personally speaking, I’ll simply talk with them about it. And I’ve heard other staff do it as well.…
I’ll hear a patient say, “I need a phone. I’ve got to tell my crew to — ” whatever they need to do ... and I’ll say to the person, “Let’s hold off on that. We’ve got some more tests to do— ” or something like that.
If they push, then it’s simply a conversation like, “I want you to really think about what you’re saying.” And then there’s still a lot of anger, and I try to make it as human as I can. “Let’s say you get that guy. What happens to his mom? What happens to his children — if he has any? What happens to his family?” I try to frame it like that. “You were almost killed. Imagine how your mom would have felt, imagine how your family would [have felt]....”
I don’t know if it’s had success or not…. A guy last week I saw, by the end, was just incredibly apologetic. His family was in and he was apologetic and crying ... and praying with them.
By the end, he told us he was going to go be a minister and stuff.... I don’t know where that went, but it was certainly an interesting reaction.

Andrew Gill/WBEZ
The worst part of the job
Adrian: A lot of times, a lot of people show up [to the hospital]. These are young folks with a lot of friends and huge social circles, and you have 30, 40, 50 people that will be in the waiting room that spills out into the parking lot…. You try to identify who the immediate family is ... and you go back [to] a family waiting room.
A lot of these people know what this means — they know the implication of what being brought back to this room means.... And you go in, and you go in with a chaplain and usually it’s a roomful of people, maybe 10 or more people.
There’s just no good way to do it. It’s like this out-of-body experience where you end up telling complete strangers the most devastating news they could ever hear…. It falls out of your mouth and then you’re just left there and the reaction is ... every different type of reaction that you could ever imagine is one that we’ve seen. You see people who are quiet and in denial. You see people who threaten us, and tell us to go back and keep working. You see people punch through walls. You see people on the floor. You see some people who thank you for trying.
The experience is, unless you’ve done it, it’s just an incredibly surreal and emotionally draining event that is just the single worst part of the job, by far.
This interview has been edited for clarity and brevity. Click the play above to hear the entire conversation.
Linda Paul is a freelance radio reporter who lives in Chicago. You can see some of her work at her website.
This story is part of WBEZ's Every Other Hour project. Find more stories here.
Criminal justice reporting and investigative journalism at WBEZ is supported in part by Doris and Howard Conant, The Joyce Foundation and the Robert R. McCormick Foundation.